Nano Masters AI Health Care Equipment
Nano Masters AI Health Care Equipment is a healthcare technology company that designs and supplies AI-enabled medical equipment for hospitals, clinics, and care providers. It focuses on integrating intelligent software, connected sensors, and data analytics into diagnostic, monitoring, and treatment-support devices to improve clinical efficiency, patient outcomes, and operational reliability.
About Nano Masters AI Health Care Equipment
Nano Masters AI Health Care Equipment is a healthcare technology company focused on building and supplying AI-enabled medical equipment for hospitals, clinics, and care providers. Its core approach combines connected sensing, embedded intelligence, and clinical-grade analytics to support diagnosis, continuous monitoring, and treatment decisions. The company designs devices and software as an integrated system: hardware captures high-quality signals, edge software performs real-time processing, and cloud services deliver dashboards, alerts, and fleet insights. This architecture is built to improve clinical throughput while maintaining reliability, traceability, and security. Across care settings, Nano Masters AI aims to reduce avoidable variation in workflows—standardizing how data is captured, interpreted, and routed to the right care team. Its solutions support earlier detection of deterioration, more consistent adherence to protocols, and better coordination between departments. Operationally, the company emphasizes device uptime and lifecycle management. Connected telemetry enables proactive maintenance, software updates, and performance benchmarking across sites, helping providers control costs while maintaining safety and compliance. With a large global workforce, Nano Masters AI supports complex deployments, training, and service operations, partnering with clinical leaders and biomedical engineering teams to ensure solutions fit real-world constraints and deliver measurable outcomes.
What we offer
AI-enabled diagnostic, monitoring, and treatment-support devices; connected sensor platforms; clinician dashboards and alerting; device fleet management and predictive maintenance; data integration services (e.g., interoperability with hospital systems); implementation, validation support, training, and ongoing service contracts.

Who we serve
Primary customers include hospitals, outpatient clinics, and long-term care providers seeking to improve patient monitoring, diagnostic accuracy, and operational reliability. Key buyers and stakeholders typically include clinical leadership, biomedical engineering, IT/security teams, and procurement, with end users spanning nurses, physicians, and technicians.

Inside the business
Delivering AI-enabled medical equipment at scale requires tight coordination across R&D, clinical validation, manufacturing, regulatory, cybersecurity, and field service. Nano Masters AI operates as an integrated hardware–software organization with strong post-deployment support.
Operating model
The company operates through cross-functional product lines that own device design, embedded software, cloud analytics, and user experience end-to-end. Development follows a regulated quality management system with design controls, verification/validation, and change management. Deployment is typically project-based (site assessment, integration, training, go-live), followed by recurring services including monitoring, updates, calibration, and maintenance. Connected telemetry feeds reliability engineering and customer success teams to prevent downtime and continuously improve models and workflows.
Market dynamics
Healthcare providers are under pressure to do more with limited staff while meeting stricter safety, privacy, and regulatory expectations. Demand is rising for connected devices that can reduce alarm fatigue, improve early detection, and provide audit-ready data. Competition spans incumbent device manufacturers, digital health platforms, and specialized AI vendors. Purchasing cycles can be long, requiring evidence of clinical value, interoperability with existing systems, and total cost-of-ownership clarity.
What changed recently (fictional)
The company has expanded its connected device portfolio and increased emphasis on fleet-level analytics to improve uptime and reduce service costs. It is also strengthening compliance-by-design practices (cybersecurity, data governance, and audit trails) to meet evolving healthcare regulations and customer requirements.
Key performance metrics (KPIs)
These KPIs reflect what leaders typically track in Health Care Equipment. Each metric connects to decisions that drive outcomes.
Decision scenarios (what leaders actually face)
The scenarios below are written to resemble realistic situations in Health Care Equipment. They’re designed for practice, discussion, and evaluation — where context, trade-offs, and escalation matter.
A new AI-assisted deterioration detection feature is ready for release. Several hospitals request immediate rollout, but clinical teams want clear evidence, IT wants minimal downtime, and quality/regulatory requires controlled change management.
What this scenario reveals
How leaders balance speed vs. safety, manage regulated change, and design evidence-driven rollouts that still meet customer urgency.
A third-party library used by connected devices has a disclosed vulnerability. Some customer sites have strict change windows, and clinical operations cannot tolerate device downtime. The company must decide how to patch quickly while maintaining auditability.
What this scenario reveals
Readiness to manage security incidents with patient safety in mind, coordinate stakeholders, and maintain compliant documentation under pressure.
Common failure points (and why they happen)
AI-enabled medical equipment can fail in predictable ways when technology, workflows, and governance are misaligned. The highest-impact failure points tend to appear at the boundaries: data quality, integration, change control, and frontline adoption.
Poor signal and data quality at the source
If sensors are misapplied, calibration drifts, or data capture is inconsistent, AI outputs degrade and clinicians lose trust. Preventing this requires robust device design, self-checks, and training aligned to real workflows.
Interoperability gaps with hospital systems
Incomplete integration with EHR/clinical messaging can cause missing context, delayed alerts, or duplicated documentation. This increases workload and undermines the value proposition.
Uncontrolled software/model updates
Pushing changes without validated procedures can create safety risks, inconsistent performance across sites, and audit exposure. Regulated change management and staged releases are essential.
Alarm fatigue and workflow mismatch
Even accurate models can fail if alerting is noisy or poorly routed. Without thoughtful thresholds, escalation pathways, and user-centered design, adoption drops and outcomes don’t improve.
Readiness & evaluation (fictional internal practice)
Readiness ensures the organization can deploy, support, and continuously improve AI-enabled medical equipment without compromising safety, compliance, or operational performance.
How readiness is checked
Readiness is checked through a combination of quality system evidence (design controls, validation records, CAPA), security posture reviews, integration testing results, service performance metrics, and role-based simulations for deployment and incident response.
What “good” looks like
Good looks like: validated end-to-end workflows (device → analytics → clinician action), measurable alert performance with governance for drift, documented change control and release management, defined incident playbooks (clinical + cybersecurity), trained field teams with standardized implementation checklists, and customer-facing SLAs consistently met.
Example readiness signals
Examples include stable uptime above target, successful integrations on first attempt, low MTTR, clear audit trails for updates, documented model monitoring with drift thresholds, consistent training completion for installers and clinical super-users, and incident response exercises completed with corrective actions closed.
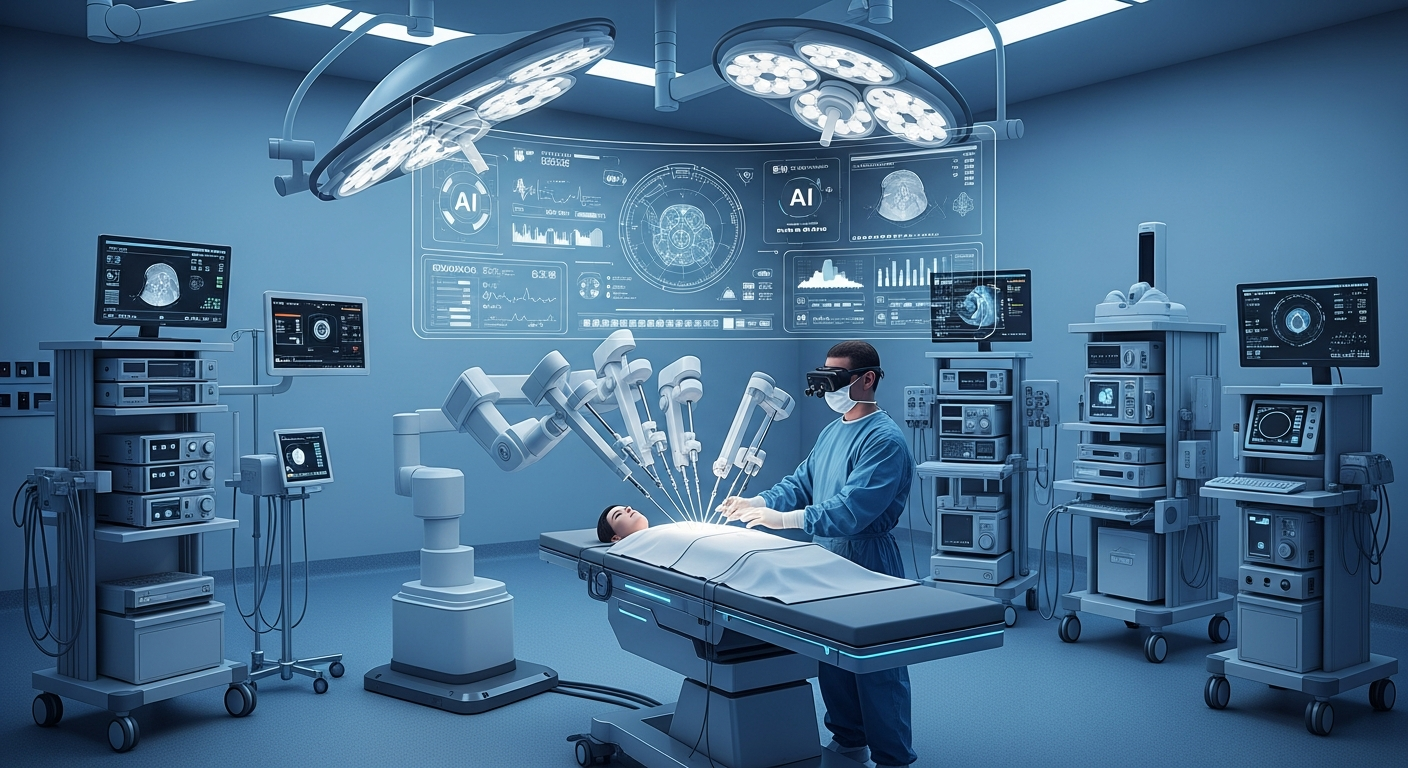
Company images
Visual context for learning (fictional, AI-generated). Three views help learners anchor decisions in a believable setting.



FAQ
Short answers to common questions related to Health Care Equipment operations and decision readiness.
What does Nano Masters AI Health Care Equipment build?
It designs and supplies AI-enabled medical equipment that combines connected sensors, intelligent software, and analytics for diagnostic, monitoring, and treatment-support workflows.
Who are the typical customers?
Hospitals, clinics, and care providers, along with stakeholders in clinical leadership, biomedical engineering, IT/security, and procurement.
How does the company ensure safety and compliance for AI-enabled devices?
Through regulated quality processes (verification/validation, change control), cybersecurity-by-design practices, audit-ready documentation, and ongoing monitoring for performance drift and reliability.
What makes connected device analytics valuable for providers?
It improves visibility into device health, supports proactive maintenance, reduces downtime, and helps standardize clinical workflows with measurable performance metrics.
Contact & information
Website: https://nanomasters.ai/blueprint-company/nano-masters-ai-health-care-equipment
Location: Netherlands
Industry: Health Care Equipment